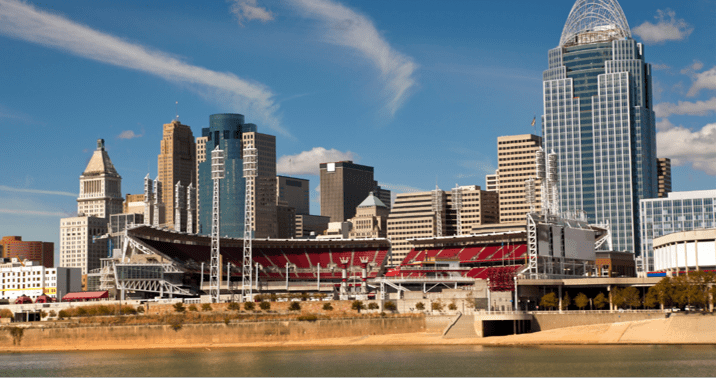
NASH, Texas, April 12, 2023 /PRNewswire/ — CSI Pharmacy, an independent, national specialty pharmacy and home infusion provider, announced today the opening of its third regional pharmacy location. Operating out of West Chester, OH, the new location greatly expands the company’s current dispensing capabilities.
“With the recent opening of our Connecticut pharmacy in February, the addition of our Ohio location positions CSI Pharmacy as a national player in the specialty infusion industry,” said COO Randy Broyles, RPh. “Multiple locations help us not only compete more effectively in local markets, but also improves our ability to secure in-network status with some regional and national insurance providers.”
“The addition of our Ohio location positions CSI Pharmacy as a national player in the specialty infusion industry.”
“It also means we are better prepared operationally in case of emergencies,” added Chief Pharmacy Officer, Jack Lemley, PharmD. “Having the capacity to shift dispensing locations in case of severe weather or other disruption means our customers have an extra layer of security with their care.”
The new state-of-the-art facility allows for complete duplication of its primary pharmacy operations in Nash, Texas. With 12,000 square feet of space, the West Chester pharmacy provides space for additional medication storage and distribution capacity, as well as a multi-chair infusion suite.
“While the vast majority of our customers are infused at home, infusion suites offer important benefits to some patients,” Lemley explained. “Those might be patients who either like the social environment of an infusion suite, require a higher level of clinical monitoring, don’t want to store their medications and supplies at home, or otherwise can’t or don’t want to bring their medical treatment home with them.”
About CSI Pharmacy
CSI Pharmacy is a national specialty pharmacy dedicated to serving patients with chronic and rare illnesses. Founded by pharmacists in 2014, the company specializes in treating rare diseases with biologics and plasma-derived therapies. It employs specially trained infusion nurses to provide these treatments to patients around the country. CSI continues to be led by co-founder and CEO, James Sheets, PharmD. Today, CSI Pharmacy is licensed to dispense in 48 states, plus D.C., and is accredited by two of the nation’s leading specialty pharmacy accrediting bodies: the Accreditation Commission for Health Care (ACHC) and URAC.
SOURCE CSI Pharmacy, LLC