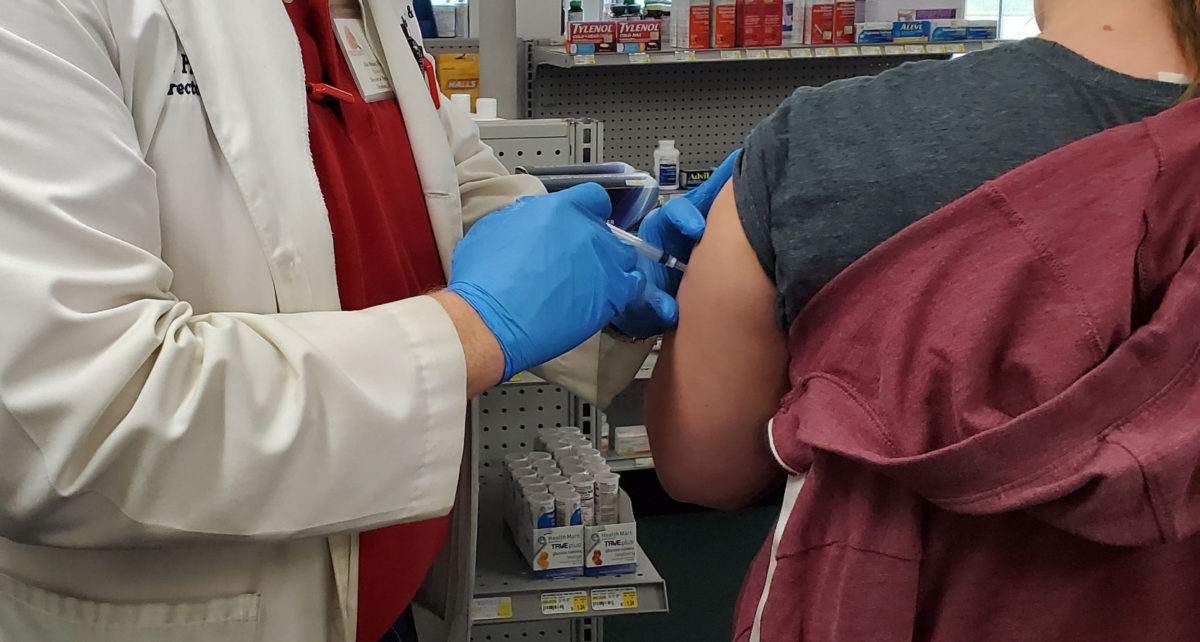
Across the country we are starting to see the light at the end of the tunnel as the rollout of COVID-19 vaccines has begun. For many of our patients with primary immunodeficiency diseases or autoimmune conditions, however, getting vaccinated is not a straightforward decision. They have lots of questions and must weigh carefully a number of considerations.
Immunologist and rheumatologist Dr. Terry Harville has some concerns, too. “There are questions in my mind that haven’t been fully answered,” he says about the new vaccines that have recently been granted emergency use authorization by the Food and Drug Administration (FDA). “And I’m worried that there will be unintended consequences.”
The fact that we have only two months’ worth of safety data from the clinical trials testing these new vaccines from Pfizer/BioNTech and Moderna leaves many medical professionals worried about longer-term effects. Others are unsure about how the vaccines will react in patients with rare autoimmune and primary immunodeficiency diseases, because testing did not include people who live with these conditions.
Despite these concerns, Dr. Harville—along with most other healthcare practitioners—stresses that most people should still get the vaccine. Because when hundreds of thousands of people get COVID and one or two percent of them die, the statistics overwhelmingly support COVID-19 vaccination.
Dr. Harville, who is a professor of medicine at the University of Arkansas for Medical Sciences and an expert in primary immunodeficiency disorders, offers some guidelines for those who are trying to make a decision about the vaccine and might be at greater risk for complications from it.
If you have a primary immunodeficiency (PI) disease, you probably already know that you need to be careful about taking immunizations, especially if they are made with live virus. The COVID-19 vaccines that are currently being administered, however, are not made with live virus. They are created from a man-made part of the virus’s genetic code called mRNA. This means they are safer for those who are unable to take live virus vaccines.
With a few exceptions, Dr. Harville says, “It is the general consensus that we don’t see any reason to not vaccinate those with primary immune deficiency diseases.”
One exception is interferonopathies, IDs associated with dysfunction in components of the immune system called interferons. Another exception is CTLA4 deficiency. These are conditions in which patients tend to develop autoimmune disorders. Dr. Harville recommends that individuals with these types of ID should probably not get the currently available COVID vaccines. While there is no data to support this at this time, there is concern among immunologists that vaccination in this group of patients may trigger an overly aggressive immune response that would be harmful. As more data becomes available, better recommendations will be forthcoming.
If you use immune globulin therapy, there appears to be no reason you shouldn’t get the vaccine. In fact, even if you get the disease, you may actually be better off than others.
“What’s interesting is,” Dr. Harville says, “if you look at SARS-CoV-2 infection in patients with antibody deficiencies—whether that’s X-linked agammaglobulinemia (XLA) or common variable immunodeficiency (CVID)—when these patients are receiving appropriate immunoglobulin (IG) replacement therapy, they tend to have milder disease.”
Intravenous immunoglobulin (IVIG) has even been used, in some cases, to treat COVID-19 infection. While clinical trials to prove effectiveness are still ongoing, some physicians believe IVIG does decrease the risk of severe complications. IG manufactured from the plasma of people who have recovered from COVID-19 infection is also being tested as a treatment.
If you have had a severe reaction to immunizations in the past, this may be a reason to opt out of getting the COVID vaccine. This includes those who have a primary immunodeficiency disorder and developed the infection after receiving a vaccine. It also includes autoimmune disease patients who have experienced a severe flare of their symptoms after a vaccination.
In the 1976, there was a rise in cases of the autoimmune condition known as Guillain-Barré syndrome (GBS) that was thought to be triggered by the swine flu vaccine given that year. This was an inactivated virus vaccine, not the type of mRNA vaccine we now have with COVID. Nevertheless, if you’ve had GBS in the past, be sure to let your healthcare provider know this, as it may be a consideration for whether or not you should get the COVID vaccine.
During the COVID vaccine clinical trials, a very small number of participants who received the Pfizer vaccine developed a severe, life-threatening allergic reaction. Since then, others have also had what is called an anaphylactic response soon after getting vaccinated. If you have ever experienced shortness of breath, tightening in the throat, swollen lips or face, or other severe allergic symptoms, you should probably not get this vaccine in particular. (Other vaccines using whole virus are currently in development and will likely be safer.) Anyone who does get a COVID vaccine should be observed for at least 15 minutes and be sure the healthcare personnel administering it have emergency equipment needed to respond to anaphylaxis.
Regardless of your disease, everyone can reduce their own risk. Dr. Harville stresses that, even if you get vaccinated, it’s still important to wear a mask, wash your hands, and maintain physical distance from others.
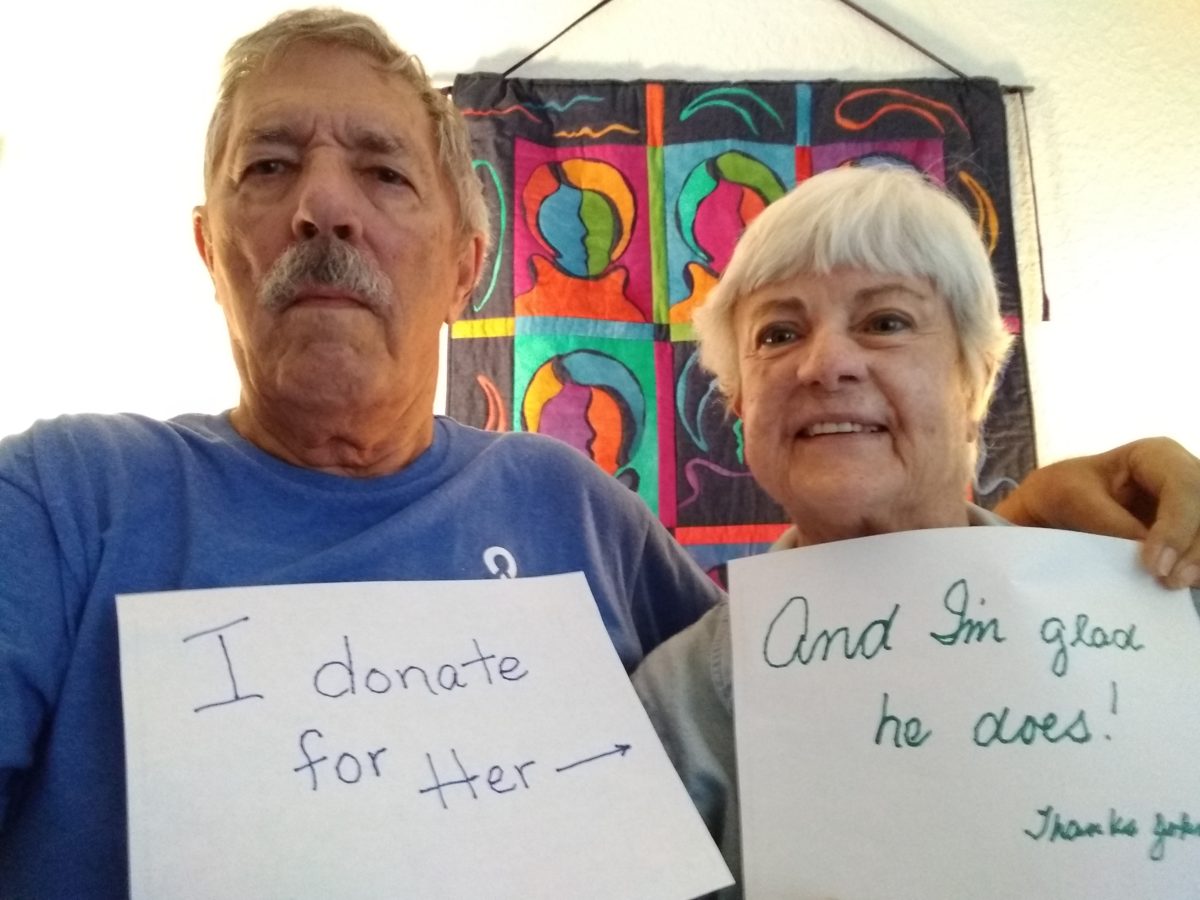
“Ultimately whether you take or do not take the vaccine is an individual patient decision,” Dr. Harville says. “This should be made after weighing all the risks and benefits and based on a discussion with your physician.”
We highly recommend that you learn more about the risks and benefits of COVID-19 vaccination as it relates to your particular situation. The Centers for Disease Control and Prevention (CDC) offers these guidelines for COVID-19 vaccination for those with underlying medical conditions. In addition, a number of disease organizations offer educational programming about the impact of the virus and the vaccine on specific disease conditions.
Please also see disease-specific statements about COVID-19 vaccines from these patient organizations:
Guillain-Barré syndrome – GBS|CIDP Foundation
Immune Deficiency Foundation
Myasthenia Gravis Foundation of America
The Myositis Association
Myositis Support and Understanding
Platelet Disorder Support Association